 Did you know that around one third of our population are living with Non Alcoholic Fatty Liver Disease? You may be wondering what is Non Alcoholic Fatty Liver Disease (NAFLD) or how do I know I have it, or what can I do to prevent it? Nonalcoholic fatty liver disease is an umbrella term for a range of liver conditions affecting people who drink little to no alcohol, or less than 2-3 standard drinks per day. As the name suggests, the main characteristic of NAFLD is too much fat stored in liver cells. Here we will discuss what NAFLD is, what causes NAFLD, and what you can do to reverse NAFLD. How common is NAFLD in Australia? It is estimated that around 30% of the Australian population has NAFLD, with this number increasing to around 75% in people who are obese or have Type 2 Diabetes. What causes NAFLD? NAFLD is generally linked to overnutrition, and is strongly associated with
What are the symptoms of NAFLD and how is it diagnosed? NAFLD generally does not cause any symptoms until it progresses to a more advanced form of liver disease, therefore most people do not know that they have the condition unless screened through blood tests or incidental findings through ultrasound. To accurately diagnose NAFLD, an ultrasound or biopsy is performed. What are the health consequences of NAFLD? Individuals with NAFLD have a higher prevalence of coronary heart disease, cerebrovascular disease, such as a stroke, and peripheral vascular disease, with cardiovascular disease being the leading death of patients with NAFLD. And their risk for cardiovascular disease is independent of any other risk factors for CVD such as stress, smoking, inactivity, etc. What is the treatment for NAFL? The first line treatment for NAFLD or any liver disease is lifestyle changes and therapy. This may occur in conjunction with medication management of the person’s other conditions such as diabetes, hypertension or high triglyceride levels. What forms of lifestyle therapy are beneficial? Weight gain is a major determinant of NAFLD, therefore weight loss is a key goal of treatment, with as little as 2-3% reduction in body weight causing a reduction in liver fats by as much as 20-30%. However the most benefit and possible reduction of NAFLD is seen with 7-10% of body weight losses. When looking at the research, neither exercise nor nutrition efforts alone are the most effective, but a combination of both have been shown to have the best effect on weight loss. However, further research has demonstrated that reductions in liver fat%, along with improvements in other health factors such as triglyceride levels, blood pressure, body fat percentage and improvement in fitness, leading to a reduction in CVD and all cause mortality can be achieved through exercise, independent or regardless of weight loss. Therefore exercise is a key component of successful treatment of this condition. What exercise is best in treating NAFLD? There has been various research looking at both aerobic exercise and strength training in the treatment of NAFLD, with aerobic exercise being superior and recommended. In terms of type, frequency, time and intensity of that aerobic exercise, there have been benefits shown for both moderate and vigorous intensities of varying durations. However the general rule is to: Accumulate 150–300 min per week of moderate‐vigorous‐intensity aerobic exercise, on at least 3 days of the week. This could include walking, cycling, running, cross trainer, swimming, type activities raising your heart rate to a minimum moderate level. It has also been shown that increasing your intensity and heart rate to higher levels further benefits for your fitness, reduces blood glucose levels and decreases your risk of mortality; and may have better effects in reducing liver fat for people with more advanced liver disease beyond NAFLD. Lisa Parkinson Accredited Exercise Physiologist & Credentialled Diabetes Educator.
1 Comment
 85% of shoulder pain in primary care is sub acromial, so, if you have ever had unexplained shoulder pain it is likely to be subacromial shoulder pain. This term is not a specific diagnosis however is commonly used by health professionals. Other names that you may have heard are subacromial impingement syndrome, subacromial shoulder impingement, or just shoulder impingement. If you have ever suffered or been told your pain is subacromial shoulder pain and you're unsure what it is and how to help it, let me help you! We will nut this out together! What is Subacromial Shoulder Pain? The word subacromial refers to the space between the top of the arm (humorous) and the pointy bit of your shoulder (acromion). Refer to the picture below to help you. Within this space, important shoulder muscles run, you may have heard of the rotator cuff, or more specifically supraspinatus (one of the rotator cuff muscles, there are 4). Another structure that is within this space is a bursa, a fluid filled sack for cushioning and comfort of the rotator cuff. The pain you experience is due to some form of irritation of these structures within the subacromial space. This irritation can begin from a traumatic event such as grabbing something really fast and wrenching on your shoulder or from overusing the shoulder, when the shoulder is worked more than its capacity can handle. People who commonly get this shoulder pain are people who do some DIY gardening or home renovations and particularly when they are with overhead movements. Often the cause of your shoulder pain is a combination of overusing the shoulder and poor shoulder mechanics. The common diagnosis you may hear are;
Whatever the mechanism, the structures of the subacromial space become inflamed and cause pain. Management of Your Shoulder Pain You may find yourself going down many different pathways to manage your shoulder pain with different health professionals however some have been found to be more effective to others. Specific exercise to improve shoulder strength and function have been found to be very effective for subacromial shoulder pain. Treatments that are often seen for this type of pain include:
Activity modification and exercise have been the most effective in producing long term success in improving shoulder pain. Below we will go through management for improving shoulder pain Unloading the shoulder or modifying activity We have to take steps to modify whatever is irritating the shoulder. What movements are hurting your shoulder at the moment? What movements help your shoulder pain? What things do you do to relieve pain? When is your shoulder pain the worst? These are all the questions we need to answer so that we can modify the activity we are doing and unload that shoulder and settle down your pain and get you back to the activities you want. Loading up the shoulder I know what you're thinking, I've just told you to unload the shoulder! However we also need to find a load that the shoulder can handle so we can reduce the amount of strength lost meanwhile building up specific shoulder strength. Not to mention there are certain exercises that have shown to have a reducing effect on pain. As I said above, often the cause of your pain is from overuse and poor mechanics, therefore it is important that we target improving the mechanics of the shoulder and build up the strength of the shoulder so it can handle a higher capacity. Loading up the shoulder is a gradual process, the trick is to find the right starting point and progress as our body adapts so that we avoid the best we can flare ups of pain along the way. Flare ups, however are common and sometimes unavoidable, however doesn't mean we are doing damage to our body. There are certain types of muscles that we aim to target in the initial phase of shoulder rehabilitation to improve shoulder mechanics and strength and these include; Rotator cuff muscles: The rotator cuff muscles are important for shoulder stability and strength. The job of these muscles is to rotate the Humerus (upper arm) both internally and externally, however their arguably more important role is to hold the head of the upper arm in the socket of the shoulder. By improving the strength and durability of these muscles we can help improve the stability of the shoulder particularly when it is moving. Below is an exercise targeting rotator cuff muscles. Muscles that move the scapula (shoulder blade): As the upper part of the arm (humerus) is joined onto the scapula at the glenoid fossa, the muscles that move the scapula have an important role in keeping the glenoid fossa in the correct place for shoulder movement. Not to mention the movements the scapula can do help to improve the subacromial space. Below is an exercise targeting the muscles that move the scapula (shoulder blade). Muscles that adduct the Arm (bring the arm towards the body): These muscles are important as when you lift your arm above your head, naturally the muscles of your shoulder are pulling the upper part of your arm (humerus) upwards towards the acromion (pointy bit in your shoulder) reducing the subacromial space. Essentially the adductors of the arm help to pull the upper part of your arm (humerus) towards the ground. Below is an exercise targeting the muscles that adduct the arm. You may be wondering, I've got all this great information and some exercises I can try! How long will it take before my shoulder pain will go away and I can start to do what I want? That questioned cant be answered on here as shoulder recovery is very individualised however research has shown that people with shoulder pain typically don't start to feel improvement until up to 6 weeks and it can take 12 weeks or longer before they can get to a satisfied outcome. Key takeaways from this Blog are:
Don't be alarmed! It's better to take 12 weeks then to have ongoing pain for years. If you have read this blog and still don't know where to start, come in and see one of our exercise physiologists. The videos shown are just some examples of baseline exercises and may not be the right exercise for everyone. Izaac Boylan Accredited Exercise Physiologist 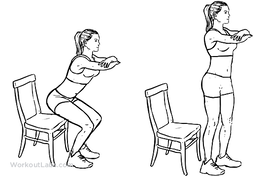 Osteoarthritis is the leading cause of hip and knee replacements in Australia, with every 1 in 11 people having some form of Osteoarthritis. Strengthening the muscles around the knee joint can decrease the load put through the joint and as a result decrease pain levels and stiffness. But… What are the best exercises to be doing to achieve this? 1. Squat (to chair) Completing a squat or modified squat to a chair is a fantastic way to build strength in the quadriceps, hamstrings and gluteal’s which all sit above the knee joint. Start by sitting on a chair with your feet on the ground, hip width apart and crossing your arms over your chest. Begin squeezing through the bottom and push yourself upright to be standing, once at full extension, begin slowly lowering back down to the chair. Try starting with 2 sets of 10 repetitions and building up from there. 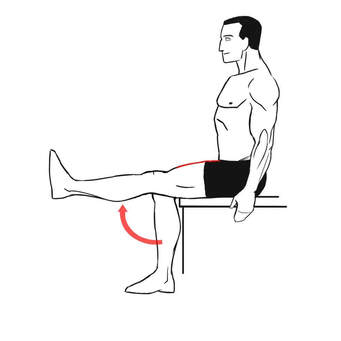 2. Seated knee extension A knee extension focuses predominantly on strengthening the quadricep muscle at the front of the thigh. Begin by sitting in a chair with your feet just slightly off the ground. Start with the right leg and straighten your leg out fully, before slowly lowering the leg back down to a bent knee position. Swap to the left leg and complete the same movement. To increase the difficulty of the exercise try adding ankle weights or a resistance band attached to the back leg of the chair to further build strength in the quadricep. Begin with 2 sets of 12 repetitions on each leg and gradually increase. 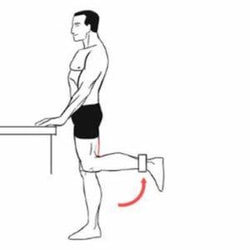 3. Standing knee flexion Knee flexion is the opposite movement of knee extension which involves bending at the knee to strengthen the hamstring muscle at the back of the thigh. Start in a standing position near a wall or bar for support, then shift your weight to your right leg, begin to bend your left knee, bringing your heel up towards your bottom, before slowly lowering back down to the ground. Swap to the right leg and repeat. To increase the difficulty of the movement, add some ankle weights or attach a resistance band to something stable in front of the feet to further progress strength in the hamstring. Begin with 2 sets of 12 repetitions on each leg and increase slowly.  4. Step ups Step ups provide many benefits to not only knee osteoarthritis but also improving overall function and stability of the pelvis and legs. Step ups assist in developing not only lower limb strength but also balance too. Start with a low step and firstly place your right foot up onto the step followed by your left foot. Then return your right foot back down to the ground first, followed by your left foot. Ensure that your knees are tracking over your feet/ toes when stepping up and down off the step. Begin with 2 sets or 8 repetitions on each leg and increase both the height of the step and the number or sets and repetitions to continually improve. If you experience knee osteoarthritis or would like to improve your overall lower body strength and joint function, give these 4 exercises a go at home. If you have any further questions about knee Osteoarthritis or how exercise can assist in decreasing pain levels, please email us at [email protected]. By, Aleisha Michael. Accredited Exercise Physiologist  Why is Exercise Important Exercising throughout any stage of your cancer journey is an important part of the fight against cancer. Exercising before treatment can reduce treatment complications and enhance post treatment recovery, exercising during treatment can reduce the amount and severity of treatment related side effects and exercising post treatment can decrease the risk of recurrence, aid in recovery and decrease the amount and severity of treatment related long term side effects. Benefits of Exercising with Cancer Exercising can improve:
Exercising can reduce:
Is Exercising with Cancer Safe In general, exercise is considered safe for those who are or have been through cancer treatment when commenced at an conservative starting point, progressed gradually and modified appropriately to accommodate for treatment and disease related side effects and co-morbidities. Cancer and cancer treatment can affect your ability to exercise in many different ways, including:
It is important to identify and consider these changes in your ability to exercise when starting an exercise program. What Type of Exercise is Best It is recommended to engage in 150+ minutes of moderate intensity activity a week or 75 minutes of vigorous intensity exercise per week. It is also recommended to do 2 resistance training (muscle strengthening) sessions a week . To get additional health benefits, engaging in anywhere up to 300 minutes of moderate intensity activity a week is preferred. Some exercise is good, more is generally better, however everyone starts at different stages. Some general rules for exercising with cancer:
The most important aspect of an exercise program for any cancer fighter or survivor is that their program is individualized to their needs, capacities and preferences. If you are going through or have gone through cancer treatment and have any questions regarding this post and want to begin to exercise, consulting an Exercise Physiologist is a great way to start. Izaac Boylan Accredited Exercise Physiologist  What is pre-diabetes? Pre diabetes is a condition when a person has blood glucose levels that are higher than normal, but not high enough to be diagnosed with type 2 diabetes. There are two types of pre-diabetes conditions:
Do people experience symptoms with pre-diabetes? Generally most people do not experience symptoms with pre-diabetes or they are so slight that they do not notice them. Pre Diabetes is the precursor to Type 2 diabetes, which is often called a ticking time bomb or a silent killer, as many people do not know they have the condition. It’s estimated that around two million Australians have pre-diabetes, with one in three people with pre-diabetes going on to develop type 2 diabetes. If we have pre-diabetes, what can we do to prevent ourselves from developing type 2 diabetes? We can help to manage our pre-diabetes and reduce the risk of developing type 2 diabetes and heart disease by making healthy lifestyle changes. These include:
What exercise is recommended for someone with pre-diabetes? Regular exercise can help to manage your weight and also help to reduce your blood glucose levels; and help to manage other risk factors such as blood pressure and cholesterol levels. The Australian guidelines suggest that all Australians undertake 30 minutes of planned moderate intensity aerobic exercise on at least 5 days of the week. So this could include walking or swimming, or could involve sports such as tennis and squash. The 30 minutes on 5 days a week is the bare minimum recommended, as evidence has found that better health outcomes are achieved by increasing your exercise up to 60 minutes a day. In addition to the aerobic exercise described above, undertaking some form of resistance training where you are using your muscles and working them to fatigue twice a week is also recommended, as this will help to improve your insulin resistance, and thereby reduce your blood glucose levels even more. If you are new to exercise, chatting to your doctor or local Exercise Physiologist is a great place to start to ensure you are safe to exercise and they can guide you on the right exercises for you. Lisa Parkinson Accredited Exercise Physiologist and Credentialled Diabetes Educator |
AuthorSLisa Parkinson Archives
July 2024
Categories
All
|

 RSS Feed
RSS Feed