|
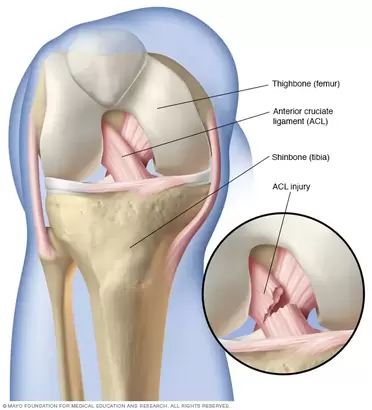
An ACL injury can be a really horrible injury and happens a lot in contact ball sports but can also happen not participating in sport. After an ACL injury more than likely you would go see a doctor ( maybe a sports doctor) and there is a good chance he will do some tests on you around your knee to inform the course of action from there. If there is a suspected ACL injury you will be sent for some imaging to confirm the doctor's thoughts. There is more than one course of action for you to take and this is dependent on your goals and what you want to get back too, this is for you and your doctor/surgeon to discuss. We now know that an ACL reconstruction immediately following an ACL injury does not necessarily mean a better outcome furthermore surgery may not be the answer in individual cases as a favourable outcome can be achieved without surgery. Not to mention the option or ability to have surgery after trying rehabilitation alone first. As EP’s we can work with physios and the treating doctor or surgeon to provide care and a path for rehabilitation back to what you love doing! What is the ACL and ACL injury? The ACL is a ligament in the knee that provides crucial stability to the knee joint. As seen in the picture below it is in the middle of the knee attaching from the thigh bone to the shinbone. The ACL prevents the shinbone from moving forward on the thigh bone. An ACL injury is a tear/rupture or strain of the ligament from some form of forceful impact that strains the ACL more than its current capacity. Other injuries commonly happen with an ACL injury, some examples of these may be meniscus injuries, trauma to cartilage, some bone trauma, injuries to other ligaments and some trauma to the joint capsule itself. These other injuries also affect injury prognosis and rehabilitation. Rehabilitation A major factor in ACL rehabilitation is that the process should be outcome based, rather than time based. This means the progression should be based on achieving outcomes that we understand mean readiness for the next phase. This means that specific and valid outcome measures are being used to track progress and guide rehabilitation. Furthermore the program for rehabilitation should be specific to the injured person, everyone's injury is different, everyone responds differently to treatment and everyone has different goals they want to achieve following injury or surgery. Phases of ACL rehabilitation There are 5 phases of general ACL rehabilitation:
Returning to sport? A more sport specific rehab protocol is the Melbourne ACL Rehabilitation Guide 2.0, this protocol was created by specialist sports physiotherapists that have worked with Olympic teams and elite AFL, netball, soccer and rugby teams, they also do research in the knee rehabilitation space. This guide is very specific and is outcome based and can be tailored to individuals and their goals. The Melbourne ACL Rehabilitation Guide 2.0 is similar to your general ACL rehab however they have included a return to sport phase which essentially assesses your readiness to return to sport both physically and psychologically. The phases are: Pre op, Phase 1 - Recovery from surgery, Phase 2 - Strength and neuromuscular control, Phase 3: Running Agility and landings, Phase 4: Return to sport, Phase 5: Prevention of reinjury. When is the best time to see an Exercise Physiologist (EP)? Well technically speaking you can begin rehab with an EP for the initial phases of treatment and throughout the whole rehabilitation process. This should be dependent on the experience of the EP dealing with ACL’s and known knee injuries.
However I would suggest seeing a physio for the early phases of rehab as generally they have more experience around ACL and acute knee injuries as acute muscle and joint injuries is what they specialise in. The best time to see an EP I feel would be either at the intermediate phase or the late phase of rehab, or somewhere in between. EP’s are well equipped to apply principles that govern strength and conditioning and apply these to rehabilitation as this is an EP’s role in musculoskeletal conditions or injuries. After all, the late phase and prevention phases of ACL rehabilitation are primarily strength and conditioning. This would all depend on the individual and the treating physiotherapists preference. All I will say is make sure you are getting sufficiently challenged and measured throughout the entire process and in particular the late stages. ACL rehabilitation is a long process, a long wait to get back to sport or the activity you enjoy! So make sure the process is worth it, you minimise any complications and reduce the risk of a re - rupture! If you need any help with your rehabilitation or want to know more please ask! Izaac Boylan Accredited Exercise Physiologist.
0 Comments
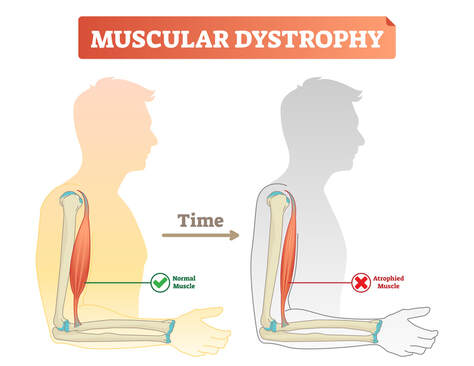
What is Muscular Dystrophy? Muscular dystrophy (MD) is a collection of diseases that cause progressize loss of muscle mass and weakness. It occurs when mutated, abnormal genes disrupt the production of dystrophin, a protein that is needed to build muscle tissue. There are many different forms of MD and unfortunately there are no known cures. The main symptom that is present across all forms of MD is muscle loss and weakness over time, although the age and specific muscle groups this begins in, varies greatly. There are several types of MD, but the most common is Duchenne Muscular Dystrophy, it occurs predominantly in males and symptom onset will usually begin in early childhood. The most common symptoms include;
Effects of Muscular Dystrophy It has been reported that people with MD lose 11-55% of their muscular strength, when compared to those without MD. As the essential protein Dystrophin is absent, it means that muscle tissue cannot repair itself to rebuild, having severe consequences on their overall health long term. Some of these long term effects can include;
How can exercise help?
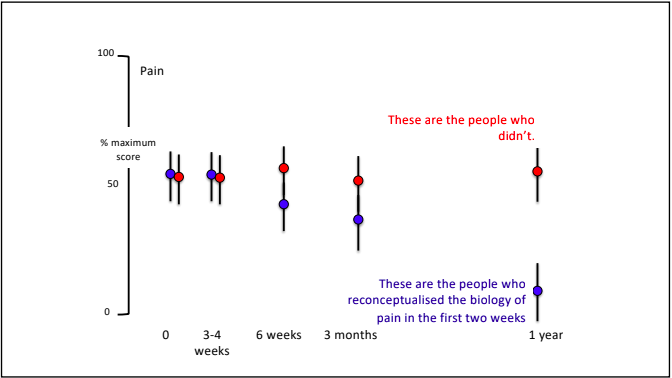
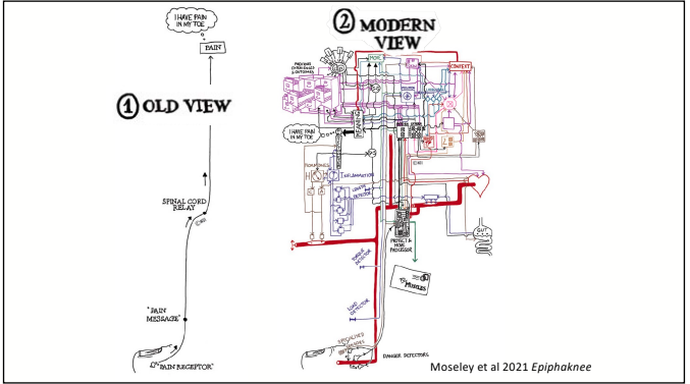
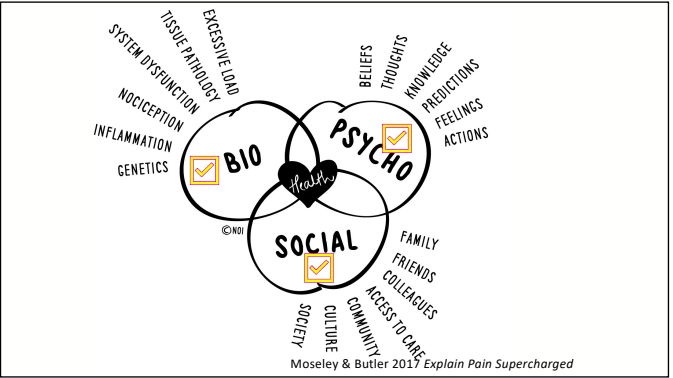
Exercise is an effective and accessible treatment option for people with MD. Tailored and specific exercise prescription is safe and can help to counteract muscle loss through increased strength and muscle mass. This assists in delaying the progression of MD and maintaining independence and physical function long term. Exercise has been shown to; increase joint stability, coordination, balance, muscular strength and endurance, fatigue levels, quality of life and mental health. It is recommended to seek exercise therapy as early as possible once diagnosed with MD. What type of exercise is best? For aerobic based exercise low impact and low intensity forms are best. This could include gentle walking, cycling or swimming, focusing on keeping them at a low-intensity level. To use a simple guide, if completing aerobic exercise with MD you should be able to hold a conversation without becoming breathless, if you are not able to, you are most likely working too hard. For strength training low load and high repetition should be the focus, starting small and very gradually building up. As muscle mass and strength will not increase at the same rate as those without MD it is important to not overdo it with strength training. Stretching is also beneficial for maintaining joint range of movement and preventing stiffness. Being mindful to not over extend through a stretch as this with MD can be hypermobile in some joints due to the lack of muscle mass surrounding them and adapted movement patterns. If you have difficulty stretching, having someone assist you with these movements can also be beneficial. If you would like more information about exercising with Muscular Dystrophy or to chat about seeing one of our Exercise Physiologists, please get in touch at [email protected] Written By, Aleisha Michael Accredited Exercise Physiologist. Pain education is a widely used treatment tool in the management of a variety of painful conditions. Education can be used to address some of the commonly held misconceptions around pain and can also be a helpful tool to help someone in pain understand why therapies such as exercise are suitable and recommended for painful conditions. I have touched on this subject in previous blogs however I have recently completed another course in pain management and thought I should spread the knowledge, because after all knowledge is power (and very important - see below) Pain education has grown and changed and is becoming more frequently used. While pain education is an important tool to use to combat persistent pain conditions, a more important factor for recovery is the learning and understanding taking place. Let me explain. Lorimer mosley’s slides, master sessions, 2022 See the above graph. In this study a group of people with persistent pain underwent pain education. These people were split into two groups which were; Blue - these people were able to understand the biology of pain in the first 2 weeks. And Red - These people were not able to. Effectively the groups were people who were able to learn and understand pain and the people who weren't. As you can see in the graph, at the 1 year follow up, the blue group ( people who were able to understand pain) significantly decreased their rating of pain. This tells us that even though both groups had the same pain education, it was the understanding and learning that was the critical factor in people reducing their pain. I believe in my own experience with low back pain that learning and understanding pain while going through university helped me to recover from the chronic pain I was having. What are the important things to learn to help improve this understanding? To answer this question, it is important to get the perspective of those who have real life experience of persistent pain conditions and were able to recover. Those people were asked following recovery from persistent pain states; “What do you think was the most important information for you to learn to help you recover?” Based on the answers to this question 4 essential facts were created. I have another blog talking through separate facts which are essentially squeezed into these 4 concepts. Fact 1: Pain protects us and promotes healing Pain is fundamentally a mechanism used for protection of the body. Pain is used by the body to prevent injury or damage through behaviour change. Think of pain as the body’s alarm system. If the body is in danger of injury or harm, pain will be used as a protective mechanism to stop whatever you are doing to prevent any harm. If an injury occurs, then the body will sensitise the area of injury to prevent further harm. This means pain will be felt long before there is any potential injury or harm and this allows the body to heal. Therefore pain is protecting us and promoting healing. Once the body heals, it becomes less sensitive and we can go back to normal. Pretty clever hey. Follow the video for a short explanation for what we mean by, pain protects us and promotes healing. Fact 2: Persistent pain overprotects us and prevents recovery Although pain is there to protect and help recovery from injury, unfortunately like everything sometimes it does not work the way it was intended. The sensitivity increases or remains after the injury has healed and the effectiveness of the way the body produces pain gets better during persistent pain states. This means that pain may continue after the tissue healing process has occurred. The body learns how to produce pain by strengthening neural pathways and the body is still trying to protect itself even after the injury has recovered. Why the body is still trying to protect itself is different in each and every individual and could include multiple and many reasons. Fact 3: Many factors influence pain Pain originally was thought to be just neural pathways that responded to nerve endings in the tissues of the body. When in contrast we now know that pain is an output produced by the brain which is a result of multiple different influences. The slide below shows the old view vs the new view of pain which shows just how complex pain is! Detection from the tissues in the body plays a vital role in the pain system but new research now tells us that it is neither essential nor necessary for pain to be produced. This means that feeling down, believing you should be in pain or getting told a awful story of someone who had back pain like your own can change the way the pain feels. Now. I'm not saying this is the reason for your pain but I am saying pain is individual and felt different by everyone because everyone has different contextual factors. Things that influence pain can be broken down into 5 categories;
Facts 4: There are many ways to reduce pain and promote recovery. Here is the great part. Now we know pain is influenced by a vast amount of factors, we have a larger amount of things we can target. Of course tissue health plays an important role but potentially your current health is not promoting a great environment for your body, maybe you believe the pain is with you forever and there is nothing you can do about it, or perhaps you are dwelling on past injuries and you are trying to relate those injuries with your current pain. Whatever may be influencing your pain we can target to try to promote recovery. Pain is so very complex and individual to everyone. Learning and understanding this is an important part of not just recovery but any future painful problems.
To start, have an open mind, put in some effort to learn and understand, and seek advice from your trusted evidence based practitioner. Pain is very rarely a quick fix but a journey, more than likely there will be flare ups, but that does not mean you can't move forward again. If you have any questions, please don't hesitate to ask. Izaac Boylan Accredited Exercise Physiologist |
AuthorSLisa Parkinson Archives
July 2024
Categories
All
|






 RSS Feed
RSS Feed