|
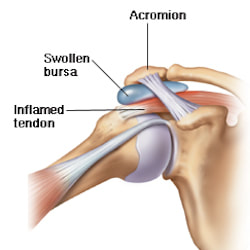
What is Bursitis? Bursitis is a condition that causes the small, fluid-filled sacs called bursae to become inflamed. A bursa is responsible for cushioning the tendons, ligaments, bones and muscles near the joint and preventing friction from occurring. This condition usually occurs in joints that are involved in repetitive movements, such as the shoulder, elbow, hip and knee. What are the symptoms? There are a range of symptoms that can present when bursitis has developed within the shoulder joint, including;
Causes of shoulder bursitis There are a number of potential causes but some of the most common can be a single injury such as a fall, repeated minor trauma like overuse injuries of the joint or muscles around the joint. When bursitis is caused from overuse injuries it is often associated with impingement and inflammation of the rotator cuff tendons as well. Prevention of shoulder bursitis Whilst it is difficult to determine singular causes in the development of bursitis there are a range of secondary factors that can contribute. Reducing causes of primary and secondary impingement are crucial in preventing shoulder bursitis and rotator cuff problems. Factors such as posture, muscle length, shoulder stability and rotator cuff strength can all contribute to the development of bursitis over time. Each of these factors can be optimised by completing specific exercises prescribed from a trained allied health professional. Treatment of shoulder bursitis
Shoulder bursitis is one of the most common shoulder injuries that presents in a range of populations. The rotator cuff muscles are responsible for the centralisation and stability of the shoulder joint. Adequate control within the shoulder then prevents injuries such as bursitis, impingement and dislocations. Interestingly, the arm only has one bony joint attachment where the collarbone meets the tip of the shoulder blade. The remainder of the shoulder joint attachment and stabilisers are all muscular, highlighting the importance of maintaining strength in the shoulder. Treatment for shoulder bursitis focuses on increasing range of movement in the shoulder joint without pain, regaining control of the shoulder blades, upper back and neck and improving strength in the rotator cuff and shoulder muscles. Each of these steps can take a number of weeks to successfully complete, so it is important to be patient and consistent during your treatment. If you suffer from shoulder bursitis, visit your local Accredited Exercise Physiologist who can help return your function and decrease pain! Written by, Aleisha Michael Accredited Exercise Physiologist.
0 Comments
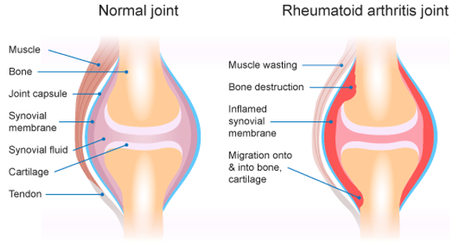
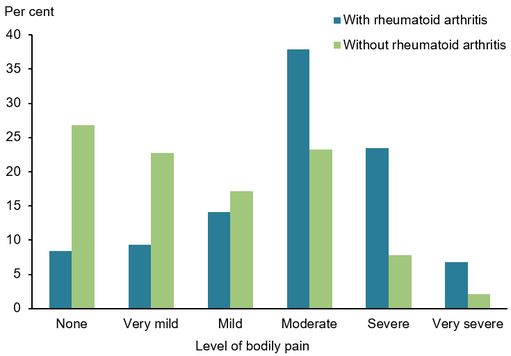
What is Rheumatoid Arthritis? Rheumatoid Arthritis (RA) is an inflammatory autoimmune disease that occurs when our immune system begins to attack its own tissue. It usually targets joints and specifically the very thin, smooth membrane that lines the joint, providing it with lubrication and nourishment. When this happens, the joint lining (otherwise known as the Synovial Membrane) can become thickened and inflamed causing potential bone erosion or growths to form. In this picture we can compare a healthy ‘normal’ joint on the left with a think layer of synovial fluid and synovial membrane surrounding the cartilage and bone, protecting the joint. In comparison on the right, we have a joint suffering from RA, with a significantly inflamed synovial membrane that is radiating into the surrounding bone and cartilage. Am I the only one suffering? You are not alone if you have been diagnosed with RA, as over 456,000 people in Australia have reported having RA and it being 1.5 times more prevalent in Women compared to Men. Data has revealed that the initial onset of RA happens most commonly between the ages of 35-64 and those over 75 years old having the highest reported incidences of RA. A study conducted by the Australian Institute of Health and Welfare that compared bodily pain levels in those with and without RA reported that in participants with RA, aged 45 and over, 68% experienced ‘moderate’ to ‘very severe pain’ in the 4-week study. This made those with RA 3.1 times more likely to experience pain classed as ‘severe’ or ‘very severe’ when compared to those without the condition What can I do to ease the pain? The good news is RA pain levels and flare ups can be significantly reduced through REGULAR AND EXPERTLY PRESCRIBED EXERCISE. We understand that it can cause anxiety and worry when exercising with RA, in fear of increasing pain within the inflamed joints BUT, research tells us that exercise is a crucial element in managing pain and flare ups. We know that movement assists in DECREASING STIFFNESS AND INFLAMMATION as it increases lubrication within the joint. Decreasing the level of stiffness within the joint will also INCREASE ITS RANGE OF MOVEMENT, providing a prolonged improvement in mobility. Regular strengthening exercise will also increase the strength of those muscles surrounding the affected joint, REDUCING THE LOAD AND IMPACT they are required to endure. As WEIGHT LOSS can be a by-product of regular exercise this can also assist in reducing the load placed on the joint, decreasing inflammation and wear and tear. Not only will regular exercise reduce your RA flare ups and pain levels, it also PROVIDES ENDLESS BENEFITS TO YOUR PHYSICAL AND MENTAL HEALTH long term. This can include preventing the onset of other co-morbidities like heart disease, lifestyle-based diabetes, obesity and even other forms of arthritis. It also improves your mental health, mood, motivation and energy levels to help get you back to doing the things that you enjoy most. Should I exercise during a flare up?
The research states that during a flare up the best practice is to rest the affected joint and COMPLETE LIGHT RANGE OF MOVEMENT BASED EXERCISES, to prevent prolonged stiffness building up within the joint. These movements should be done several times per day and pushed as far as is comfortable. Whilst gentle movements will help to reduce the overall flare up time, resistance and wights should not be used during these periods. So, what types of exercises are best? There is no one size fits all exercise program for those with Rheumatoid Arthritis and programs should be individualised and tailored to you are your specific presentation. BUT.. the best type of exercise is the one that you enjoy doing the most, as this increases your likelihood to engage in it long term. In regards to assisting with RA pain and flare ups, generally low impact movements are best suited to prevent aggravating the joint. There are 3 main goals involved in RA based exercise programs;
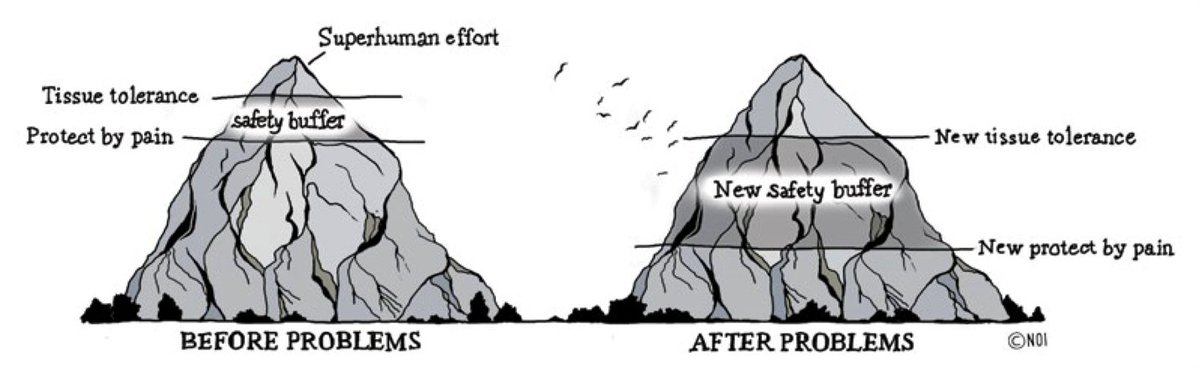
By Aleisha Michael, Accredited Exercise Physiologist. The understanding of pain has come a long way in the last 20 years and if not longer. Research on the topic has been ground breaking and has allowed us to understand pain and helped us provide better care for our clients. One area of research that is particularly interesting is around pain education and the benefits just knowing and understanding pain can have. Knowing that understanding pain can change the way your pain feels, I wanted to write this blog to give you a quick insight and understanding of some key concepts of pain to help everyone learn. Pain is always real Pain and especially chronic pain is a very complex topic, much more complex than we first thought. You may have heard stories about people who should be in pain but are not and people who should not be in pain but are, just does not make much sense right? Pain is always real, but what the contributing factors driving the pain you feel may differ. A health professional with a good understanding of pain science will never disregard your pain because they can't identify any physical reason for your pain but help you understand what may be causing or amplifying the pain you feel. Pain depends on context Pain is a complex interaction of biological, psychological and social factors. This interaction can include:
These factors that form the context of your pain may amplify or improve the pain you feel. This means the pain you feel can change just by changing the way you think and feel. Believe it or not, people have been found to have a more painful experience when exposed to heat when looking at a red light rather than a blue light because we associate red with danger unconsciously. This means a lot of factors can influence and contribute to your pain however in turn by working on changing these factors you can improve your recovery. Educate yourself on your pain The first step in recovery is to learn about your pain, this helps to understand your health professional when talking about your pain and learning about some common concepts can help you re-engage with physical activity and movement and allow you to have confidence you are not harming yourself. As mentioned previously with all the research that has been done, we now have a better understanding of what can be achieved if you know more about pain and your own pain in particular. Simply understanding pain can change the way it feels. Educating yourself about your pain helps you to be proactive and helps to take ownership of your own recovery which means you are not relying on anyone else to help you make a big difference. Pain does not always equal tissue damage The complex interaction between biological, psychological and social factors helps to understand that many factors contribute to your pain, this also helps us to understand that just because there is pain, does not mean there is tissue damage. In fact, pain is used by the body to prevent tissue damage. There is a large amount of research that has found that many people have some abnormalities on scans but have no pain and that these abnormalities are actually just age related changes. The opposite can also occur where there is pain but no abnormal changes to scans. Even the way you are told about your scans can contribute to your pain. Humans are very strong and have an amazing ability to heal or adapt. The pain experienced may be because of an acute injury or damage to tissues, but our bodies are very capable of healing, and when this pain continuous after healing, the amount of contribution of psycho social factors to the pain experienced becomes greater. When you understand that pain does not equal tissue damage, you become less afraid and more confident to move, retraining your brain system. Pain is there to protect you Pain is a deliberate and vital mechanism of the body to protect you from harm. The body uses pain to help change your behaviour that it thinks is dangerous and therefore protects you from causing any harm. The brain is at the centre of your pain system, the brain gets messages from nerves in your body that we can call “danger detectors”, these danger detectors send information to your brain that the body may be in danger. The brain then takes this information, along with all the relevant psychological and social information it has already stored and makes a decision whether your body is in danger or it is safe. If your brain concludes your body is in danger, it will produce pain in order to change your behaviour to avoid this danger. An amazing fact about the body's pain system is that it can create pain with no physical stimulus or injury. Simple thoughts, past experiences and feelings can create enough evidence of danger for the brain to produce pain. A normal pain system allows a buffer to produce pain prior to any tissue damage occurring big enough so that the injury does not happen but small enough so we don't get pain when we don't need it. This buffer grows bigger as the pain system gets more and more sensitive and overprotective because we feel pain way before our body is in danger. When your body gets over protective Like anything that happens in your body, the pain system learns pain. The more you have lived with pain, the better your pain system is at producing it. When danger messages are sent to the brain it travels to the spinal cord and then to the brain. When this process is repeatedly done, the pain system learns to respond better. This means the pain system is more sensitive and overprotective and the danger messages that are sent to the brain are turned up. When these turned up danger messages reach the brain, the brian is more likely to produce pain. The brain also gets more efficient at producing pain and the brain does not only respond to a sensitive spinal cord but also any sign of danger like from your psychological and social factors that influence pain. Resetting the buffer for your pain system to return to producing pain only when it is truly needed is an important step in getting back to your normal activities. Getting out of this the same way you got into it The reason why the pain system can become overprotective and learn how to produce pain better is because of bioplasticity. Bioplasticity is the scientific meaning of our body’s ability to adapt and thanks to bioplasticity we can retrain the pain system to return to normal. The idea of retraining the pain system starts with understanding and learning about your pain, knowing that it can be sensitive and over protective and simple things like your thoughts, beliefs and past experience can influence the pain you feel. With this knowledge you can then start to move more even when you do get some pain, eventually this movement and new belief can push the buffer of your pain system in the right direction. Resetting the pain system and its buffer takes a lot of time and patience but it is important you stick at it. Each small bit of movement is a win, each small win is remembered by your system and bit by bit you will make progress towards recovery. You are the best weapon against your pain Being proactive, looking for solutions, learning about pain, actively rethinking your own pain, trying new things and doing things for yourself rather than waiting for things to be done for you is the best way for recovery.
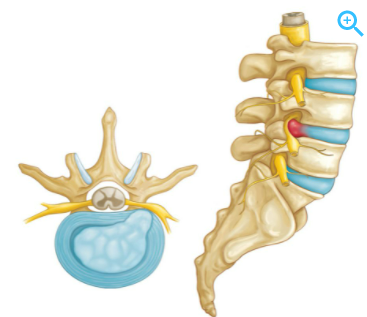
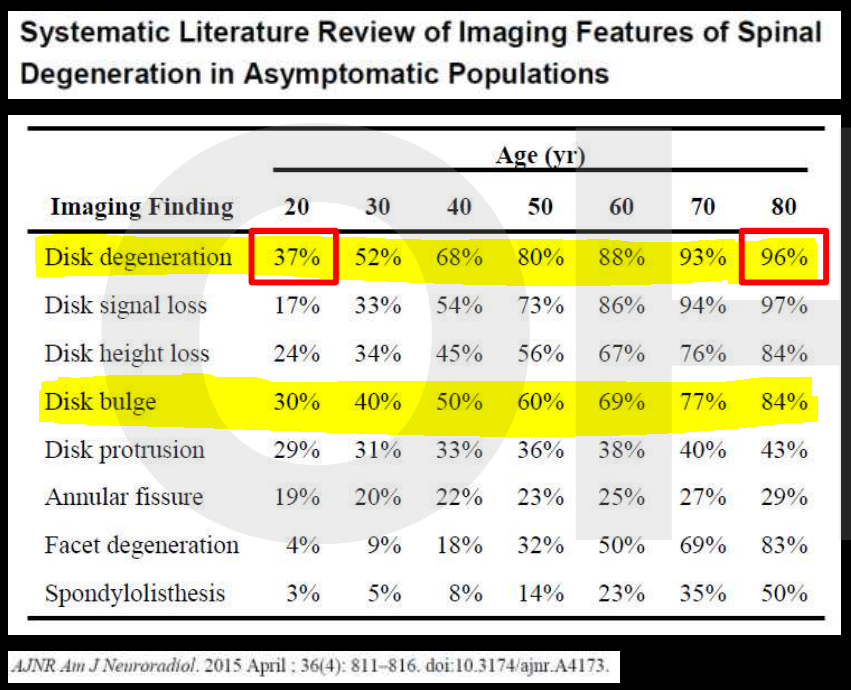
Over time you will learn more and more about your pain and what is influencing it, you will learn what the best strategies for recovery are and you will build your own positive experiences that can positively influence your pain experience. Recovery from chronic or long term pain is a journey not a quick fix. Seek the right advice, learn more about what is going on and take control. Izaac Boylan Accredited Exercise Physiologist What is a disc bulge? Did you know that almost 80% of the global population experience an episode of low back pain at some point in their life, with degenerative disc disease and lumbar disc herniation (disc bulge) being the most common. A disc bulge is also known as a bulging disc, slipped disc, or disc protrusion and is a condition during which a nucleus pulposus is displaced from intervertebral space. This can happen in the lumbar (low back), thoracic (mid back) or cervical (neck) spine. Here, the side and cross sectional views of a herniated disk are shown. In a herniated disc the soft, jelly-like centre of the disc can push all the way through the outer ring (source). This can cause pain, and may or may not press on the adjoining nerve, which can cause pain to travel down our thigh or leg, and even down to the inside or outside of our feet. Should I be concerned, will my disc bulge get better? Most occurrences of a bulging disc (disc herniation) resolve with conservative treatment and resolve within as little as two to eight weeks. 85 to 90% of cases will resolve within this time-frame and without substantial medical intervention. It can be scary when you have back pain, or have been informed you have a bulging disc, but there is really good evidence to show that it will get better, without the need for surgery. Disc Bulges - a normal part of ageing process?? Recent evidence has found that disc bulges and degenerative back conditions are a normal part of ageing, just like grey hair and wrinkles on your skin. We should not fear them as being a life sentence, rather just a normal part of life. Furthermore, they don't always result in pain. The study below shows that when 20 year olds WITHOUT back pain were scanned, 37% of them had disc degeneration, and 30% of them had a disc bulge. However, with increasing age, this number continues to increase, and in our 60's 88% of people WITHOUT BACK PAIN were shown to have disc degeneration, and 69% WITHOUT BACK PAIN shown to have a disc bulge. What should I do? Listen to your body and stay as active as you can within your own pain limits. You may find paracetamol helpful in settling your pain in the initial stages. You may find that sitting is better than standing, or vice versa, or standing and arching your back a little, or maybe even laying down and swaying your bent knees gently from side to side. Whatever movement you find that is comfortable for you, and your pain remains below a 2 out 10, continue to do. As your back starts to feel better you may be able to go for some walks, or extend your walks. Backs love movement, and the latest research now tells us that rest is not the best remedy. Deep breathing has also shown to be beneficial in relaxing the musculature of the back, helping to decrease pain. What are the long term solutions for disc bulge and back pain? Following on from the initial recovery phase, an essential part of helping back pain is strengthening and this is what Exercise Physiologists are the experts at! If we can help to strengthen your back, it is less likely that physical load will irritate it, this means that you have a decreased chance of recurrence and less severity of symptoms of future episodes. We now know that pain is multifactorial, this means there are multiple aspects that affect our pain, including psychological and social stressors, nutrition, sleep and physical aspects. We can help to assess your pain and help you to understand your pain, and the things you can do it decrease pain, and improve your strength to help you to live an active life. Discs respond to load and like getting stronger, just like muscles. It has been found that in people who run or lift weights, that their discs are stronger, fatter and healthier!! What a great reason to exercise!! We'd love to help you with your back pain!! Please get in touch or book online to book with an Exercise Physiologist who has a modern and evidenced-based approach to disc bulge and back pain. 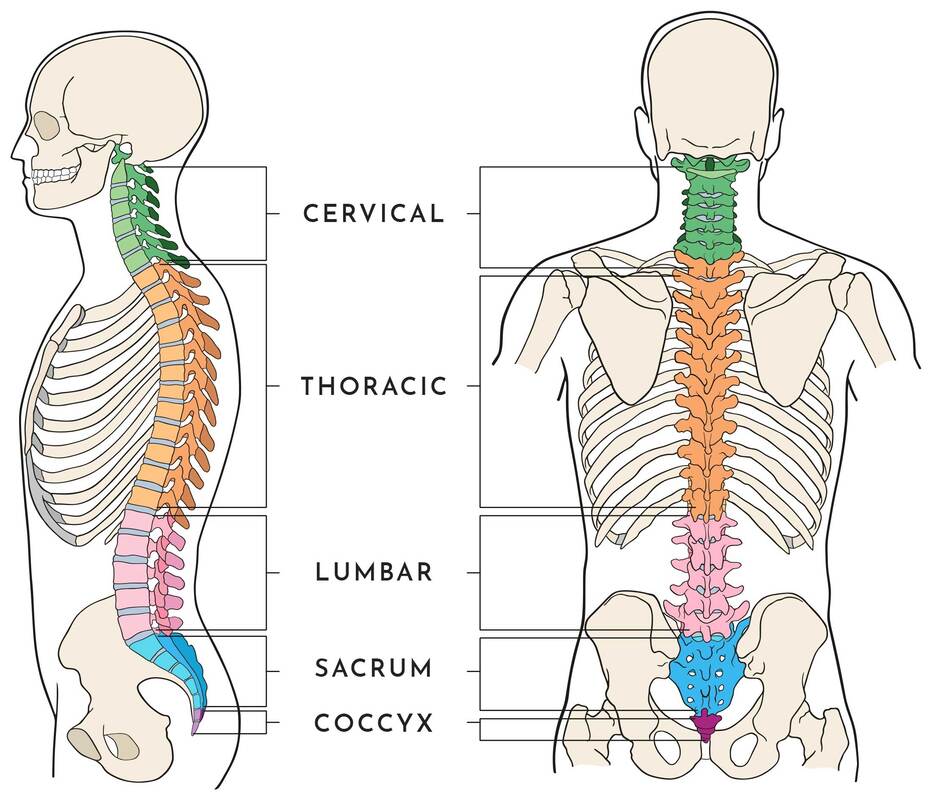 What is the thoracic spine? The spine is made of 5 different sections being the cervical, thoracic, lumbar, sacrum and coccyx. The thoracic spine starts at the bottom of the neck and ends at the abdomen and is the longest section of the entire spine. The thoracic spine consists of 12 vertebrae stacked on top of each, called T1 down to T12. These vertebrae support the neck, rib cage, connecting joints and soft tissues along with blood vessels and nerves. What is the Thoracic spine’s role in the body? The thoracic spine is crucial in supporting and stabilising the rib cage which protects all of our vital organs underneath, including our lungs and heart. It also protects the spinal cord which sends all messages and signals throughout the entire body. The spinal cord travels from the brain, down through the vertebrae before it branches off into smaller bundles in the lumbar portion of the spine. What kind of movement does it produce? The thoracic spine is not as mobile as the neck and lumbar spine and it is quite limited in forward and backward movements at the top vertebrae. Although the thoracic spine can produce more rotational movement within the top few vertebrae to help twist our chest and shoulders. Common causes of thoracic spine pain? There can be many possible causes for upper back/ thoracic pain but some of the most common include;
Common treatments Initially an increased range of movement through the thoracic spine is important to ensure that the spine can move freely without restriction. This may be done by lengthening out the muscles through the front of your chest and shoulders to enable a more upright posture to return. Increasing strength through the thoracic, lumbar and cervical spine will also assist in developing endurance to maintain an upright posture, preventing pain from returning in the future. Each case is assessed and treated individually to determine the best approach for each client. Aleisha Michael Accredited Exercise Physiologist.  85% of shoulder pain in primary care is sub acromial, so, if you have ever had unexplained shoulder pain it is likely to be subacromial shoulder pain. This term is not a specific diagnosis however is commonly used by health professionals. Other names that you may have heard are subacromial impingement syndrome, subacromial shoulder impingement, or just shoulder impingement. If you have ever suffered or been told your pain is subacromial shoulder pain and you're unsure what it is and how to help it, let me help you! We will nut this out together! What is Subacromial Shoulder Pain? The word subacromial refers to the space between the top of the arm (humorous) and the pointy bit of your shoulder (acromion). Refer to the picture below to help you. Within this space, important shoulder muscles run, you may have heard of the rotator cuff, or more specifically supraspinatus (one of the rotator cuff muscles, there are 4). Another structure that is within this space is a bursa, a fluid filled sack for cushioning and comfort of the rotator cuff. The pain you experience is due to some form of irritation of these structures within the subacromial space. This irritation can begin from a traumatic event such as grabbing something really fast and wrenching on your shoulder or from overusing the shoulder, when the shoulder is worked more than its capacity can handle. People who commonly get this shoulder pain are people who do some DIY gardening or home renovations and particularly when they are with overhead movements. Often the cause of your shoulder pain is a combination of overusing the shoulder and poor shoulder mechanics. The common diagnosis you may hear are;
Whatever the mechanism, the structures of the subacromial space become inflamed and cause pain. Management of Your Shoulder Pain You may find yourself going down many different pathways to manage your shoulder pain with different health professionals however some have been found to be more effective to others. Specific exercise to improve shoulder strength and function have been found to be very effective for subacromial shoulder pain. Treatments that are often seen for this type of pain include:
Activity modification and exercise have been the most effective in producing long term success in improving shoulder pain. Below we will go through management for improving shoulder pain Unloading the shoulder or modifying activity We have to take steps to modify whatever is irritating the shoulder. What movements are hurting your shoulder at the moment? What movements help your shoulder pain? What things do you do to relieve pain? When is your shoulder pain the worst? These are all the questions we need to answer so that we can modify the activity we are doing and unload that shoulder and settle down your pain and get you back to the activities you want. Loading up the shoulder I know what you're thinking, I've just told you to unload the shoulder! However we also need to find a load that the shoulder can handle so we can reduce the amount of strength lost meanwhile building up specific shoulder strength. Not to mention there are certain exercises that have shown to have a reducing effect on pain. As I said above, often the cause of your pain is from overuse and poor mechanics, therefore it is important that we target improving the mechanics of the shoulder and build up the strength of the shoulder so it can handle a higher capacity. Loading up the shoulder is a gradual process, the trick is to find the right starting point and progress as our body adapts so that we avoid the best we can flare ups of pain along the way. Flare ups, however are common and sometimes unavoidable, however doesn't mean we are doing damage to our body. There are certain types of muscles that we aim to target in the initial phase of shoulder rehabilitation to improve shoulder mechanics and strength and these include; Rotator cuff muscles: The rotator cuff muscles are important for shoulder stability and strength. The job of these muscles is to rotate the Humerus (upper arm) both internally and externally, however their arguably more important role is to hold the head of the upper arm in the socket of the shoulder. By improving the strength and durability of these muscles we can help improve the stability of the shoulder particularly when it is moving. Below is an exercise targeting rotator cuff muscles. Muscles that move the scapula (shoulder blade): As the upper part of the arm (humerus) is joined onto the scapula at the glenoid fossa, the muscles that move the scapula have an important role in keeping the glenoid fossa in the correct place for shoulder movement. Not to mention the movements the scapula can do help to improve the subacromial space. Below is an exercise targeting the muscles that move the scapula (shoulder blade). Muscles that adduct the Arm (bring the arm towards the body): These muscles are important as when you lift your arm above your head, naturally the muscles of your shoulder are pulling the upper part of your arm (humerus) upwards towards the acromion (pointy bit in your shoulder) reducing the subacromial space. Essentially the adductors of the arm help to pull the upper part of your arm (humerus) towards the ground. Below is an exercise targeting the muscles that adduct the arm. You may be wondering, I've got all this great information and some exercises I can try! How long will it take before my shoulder pain will go away and I can start to do what I want? That questioned cant be answered on here as shoulder recovery is very individualised however research has shown that people with shoulder pain typically don't start to feel improvement until up to 6 weeks and it can take 12 weeks or longer before they can get to a satisfied outcome. Key takeaways from this Blog are:
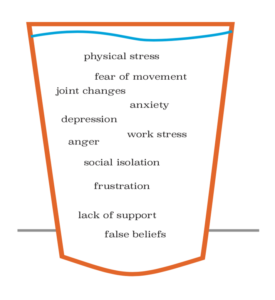
Don't be alarmed! It's better to take 12 weeks then to have ongoing pain for years. If you have read this blog and still don't know where to start, come in and see one of our exercise physiologists. The videos shown are just some examples of baseline exercises and may not be the right exercise for everyone. Izaac Boylan Accredited Exercise Physiologist Everyone has experienced pain throughout their lifetime, it is an experience produced by the brain to protect you! But when it is persistent or chronic it is not fun, however it is more than likely not tissue damage being the major factor to your pain experience. So what is driving my pain? Think of yourself as a cup If you think of yourself as a cup, and in the cup you have all the stressors in your life that may be contributing to your chronic pain. Stressors can be anything from work stress, past history with pain, anxiety, physical stress, fear of movement, false beliefs and even lack of support. When we see a lot of these stressors in our lives, the cup gets too full, it overflows and we might get pain. How Do We Stop the Cup From Overflowing? We have two options to stop the cup from overflowing, we could decrease what's in the cup or we could increase the size of the cup. Decrease What is in the Cup To decrease what is in the cup we have to identify what stressors are in the cup first and then decrease the impact these stressors are having. Some strategies to do this are:
Increase the Size of the Cup To increase the size of our cup we again have to identify what is in the cup and then develop our ability to combat these stressors. Strategies include:
So ask yourself what's in your cup? What can I decrease? or how can I build a bigger cup? To help understand pain visit https://www.youtube.com/watch?v=C_3phB93rvI Izaac Boylan Accredited Exercise Physiologist |
AuthorSLisa Parkinson Archives
July 2024
Categories
All
|





 RSS Feed
RSS Feed